Using deep learning to predict microvascular invasion in hepatocellular carcinoma based on dynamic contrast enhanced MRI combined with clinical parameters
Danjun Song*, Yueyue Wang*, Wentao Wang*, Kai Zhu*, Qiang Gao, Jian Zhou, Jia Fan, Shengxiang Rao†, Manning Wang†, Xiaoying Wang†
Journal of Cancer Research and Clinical Oncology (2021, IF=4.553)
Abstract
Purpose Microvascular invasion (MVI) is a critical determinant of the early recurrence and poor prognosis of patients with hepatocellular carcinoma (HCC). Prediction of MVI status is clinically significant for the decision of treatment strategies and the assessment of patient’s prognosis. A deep learning (DL) model was developed to predict the MVI status and grade in HCC patients based on preoperative dynamic contrast-enhanced magnetic resonance imaging (DCE-MRI) and clinical parameters.
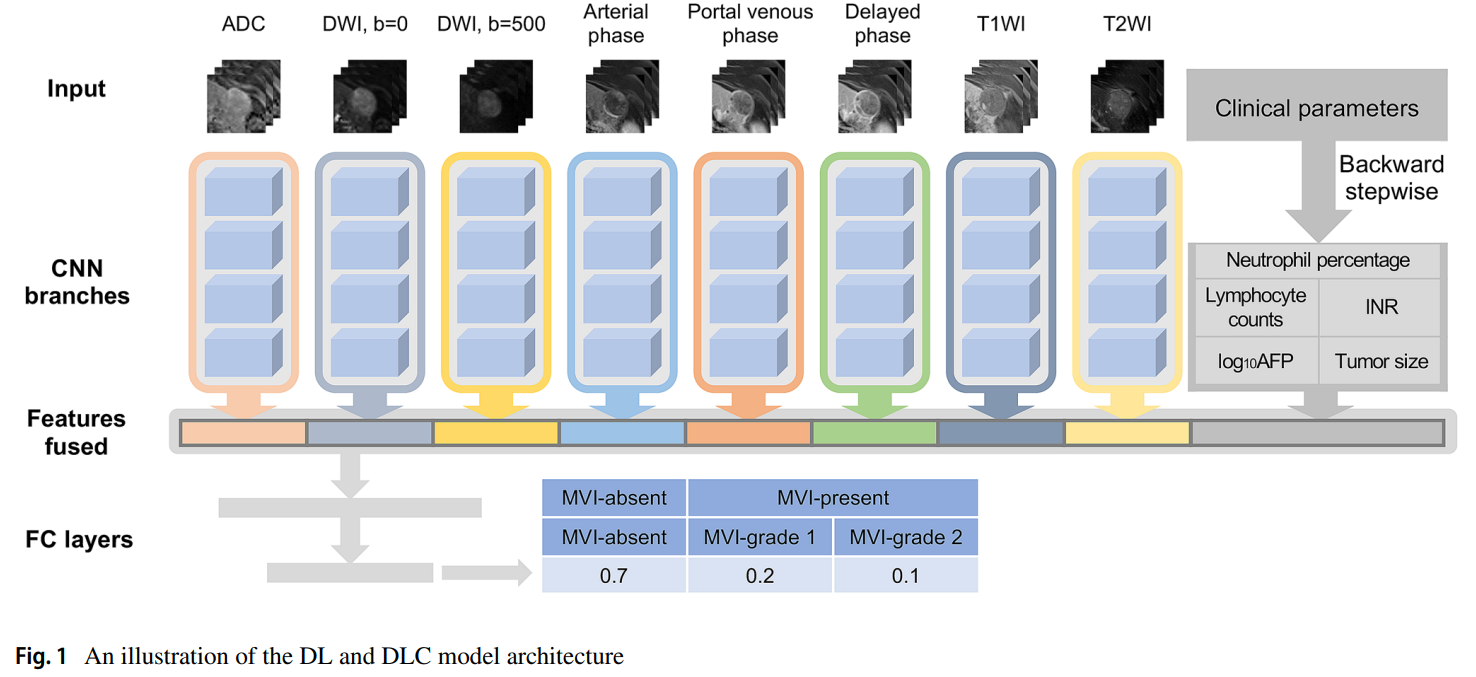
Methods HCC patients with pathologically confirmed MVI status from January to December 2016 were enrolled and preoperative DCE-MRI of these patients were collected in this study. Then they were randomly divided into the training and testing cohorts. A DL model with eight conventional neural network (CNN) branches for eight MRI sequences was built to predict the presence of MVI, and further combined with clinical parameters for better prediction.
Results Among 601 HCC patients, 376 patients were pathologically MVI absent, and 225 patients were MVI present. To predict the presence of MVI, the DL model based only on images achieved an area under curve (AUC) of 0.915 in the testing cohort as compared to the radiomics model with an AUC of 0.731. The DL combined with clinical parameters (DLC) model yielded the best predictive performance with an AUC of 0.931. For the MVI-grade stratification, the DLC models achieved an overall accuracy of 0.793. Survival analysis demonstrated that the patients with DLC-predicted MVI status were associated with the poor overall survival (OS) and recurrence-free survival (RFS). Further investigation showed that hepatectomy with the wide resection margin contributes to better OS and RFS in the DLC-predicted MVI present patients.
Conclusion The proposed DLC model can provide a non-invasive approach to evaluate MVI before surgery, which can help surgeons make decisions of surgical strategies and assess patient’s prognosis.
Paper Link: https://link.springer.com/article/10.1007/s00432-021-03617-3