Predicting Lymph Node Metastasis from Primary Cervical Squamous Cell Carcinoma Based on Deep Learning in Histopathological Images
Qinhao Guo*, Linhao Qu*, Jun Zhu*, Haiming Li*, Yong Wu, Simin Wang, Min Yu, Jiangchun Wu, Hao Wen, Xingzhu Ju, Xin Wang,
Rui Bi†, Yonghong Shi†, Xiaohua Wu†
Modern Pathology (IF = 7.5)
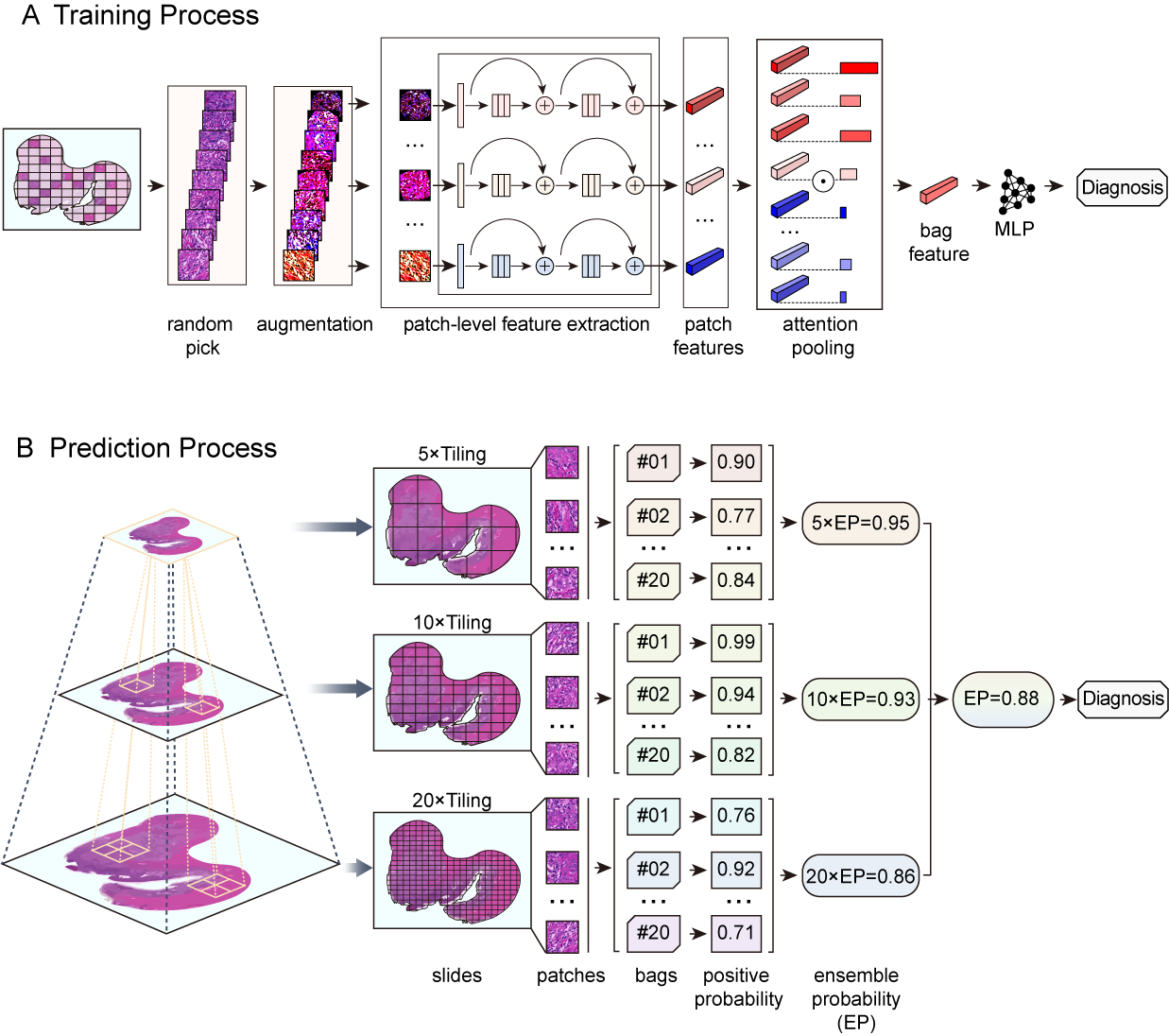
We developed a deep learning framework to accurately predict the lymph node status of cervical cancer patients based on hematoxylin and eosin (HE)-stained pathological sections of the primary tumor. In total, 1524 HE-stained whole slide images (WSIs) of primary cervical tumors from 564 patients were used in this retrospective, proof-of-concept study. Primary tumor sections (1161 WSIs) were obtained from 405 patients who underwent radical cervical cancer surgery at the Fudan University Shanghai Cancer Center (FUSCC) between 2008 and 2014; 165 and 240 patients were negative and positive for lymph node metastasis, respectively (including 166 with positive pelvic lymph nodes alone and 74 with positive pelvic and para-aortic lymph nodes). We constructed and trained a multi-instance deep convolutional neural network based on a multi-scale attention mechanism, in which an internal independent test set (100 patients, 228 WSIs) from the FUSCC cohort and an external independent test set (159 patients, 363 WSIs) from the Cervical Squamous Cell Carcinoma and Endocervical Adenocarcinoma (CESC) cohort of The Cancer Genome Atlas program (TCGA) database were used to evaluate the predictive performance of the network. In predicting the occurrence of lymph node metastasis, our network achieved areas under the receiver operating characteristic curve (AUCs) of 0.87 in the cross-validation set, 0.84 in the internal independent test set of the FUSCC cohort, and0.75 in the external test set of the TCGA-CESC cohort. For patients with positive pelvic lymph node metastases, we retrained the network to predict whether they also had para-aortic lymph node metastases. Our network achieved AUCs of 0.91 in the cross-validation set and 0.88 in the test set of the FUSCC cohort. Deep learning analysis based on pathological images of primary foci is very likely to provide new ideas for preoperatively assessing cervical cancer lymph node status; its true value must be validated with cervical biopsy specimens and large multicenter datasets.